By Andrew J. Hewitt, PMHNP‑BC
Abstract
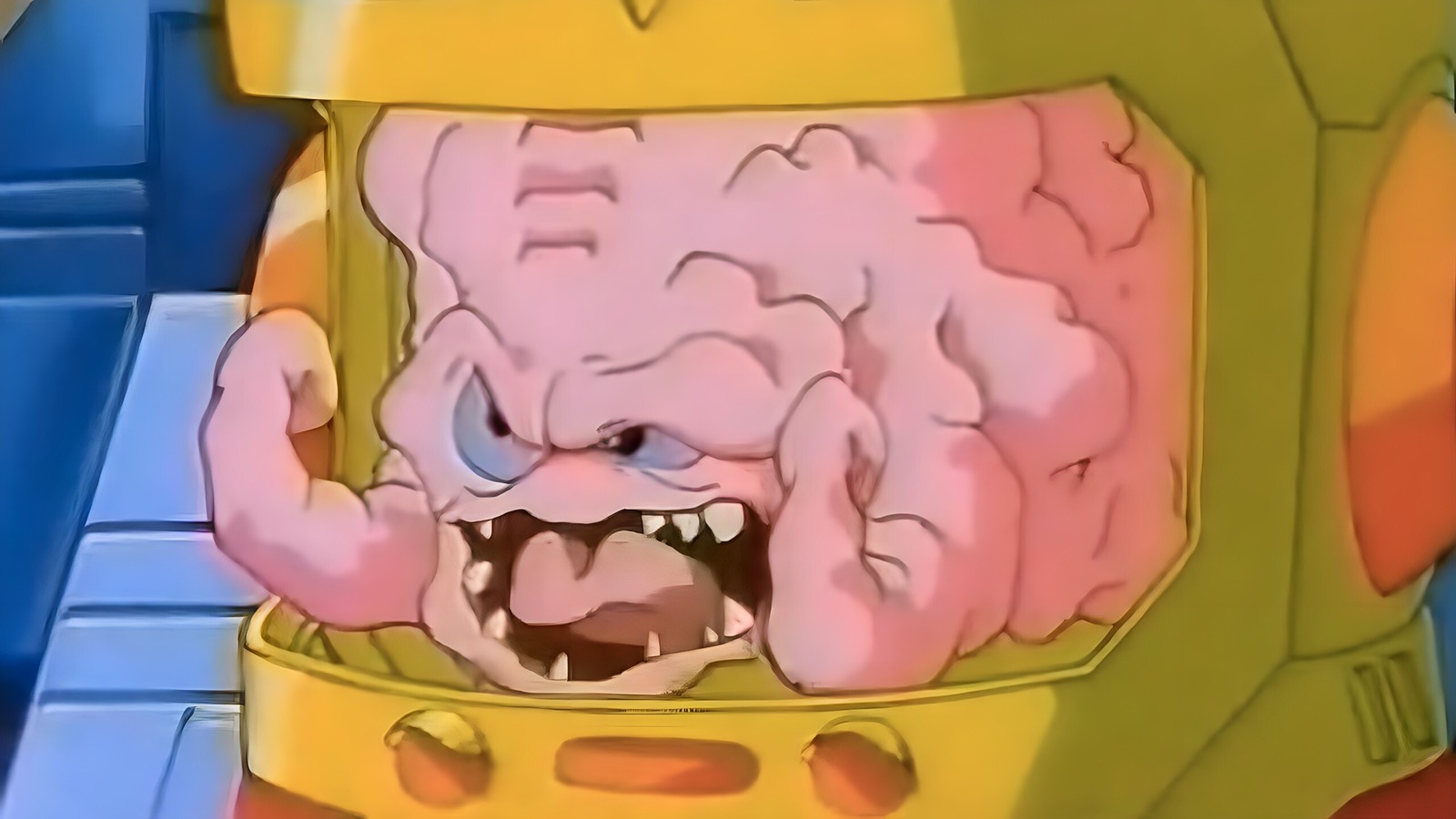
The human brain is often likened to a muscle—this analogy captures a core truth of neuroscience: the brain grows stronger through challenge, stimulation, and regular activity. Although the brain is not literally muscular tissue, it demonstrates neuroplasticity, a biologically supported capacity to reorganize itself in response to internal and external demands. Just as muscles adapt, grow, and become more efficient through strength training and aerobic exercise, the brain’s neural networks strengthen through cognitive and physical challenges that stimulate growth, connectivity, and resilience. This article explores how the brain benefits from various forms of exercise (both physical and cognitive), the mechanisms behind those effects, implications for mental health and longevity, and practical strategies for integrating brain‑ strengthening activities into daily life. The evidence—both emerging and well‑established—confirms that brains that “work out” systematically are healthier, more resilient, and better equipped to learn, adapt, and thrive.
Introduction
In contemporary discussions about health and human performance, many clinicians and laypeople alike describe the brain as a muscle. This metaphor simplifies a complex organ but remains useful: like muscles, the brain grows stronger with consistent use and stimulation. More importantly, decades of research into neuroplasticity demonstrate that the brain continues to reorganize, build new connections, and even generate new neurons in response to experience throughout life (Pascual‑Leone et al., 2025; “Neuroplasticity,” 2025). This capacity, which was once thought to diminish after childhood, persists across the lifespan and can be profoundly influenced by lifestyle factors—including exercise.
The purpose of this paper is to illustrate how engaging in both physical and cognitive “workouts” promotes brain health, improves cognitive function, supports mood regulation, and reduces age‑related decline. The goal is to bridge scientific understanding with clinical and everyday practices that patients, caregivers, and clinicians can adopt.
The Brain‑Muscle Metaphor and Neuroplasticity
The analogy of the brain as a muscle rests on the concept of neuroplasticity—the brain’s ability to reorganize itself by forming new neural connections in response to learning, experience, and environmental stimuli. Neuroplasticity supports memory, skill acquisition, emotional regulation, and recovery from injury (Pascual‑Leone et al., 2025; “Neuroplasticity,” 2025). Although the brain is anatomically distinct from skeletal muscle, its functional adaptability mirrors how muscles respond to training demands.
In muscle physiology, progressive overload leads to hypertrophy and strength. In the brain, psychosocial and physical challenges prompt synaptogenesis (creation of synaptic connections), improved efficiency across neural networks, and robust communication between regions responsible for attention, memory, and executive function (Pascual‑Leone et al., 2025). For example, cognitive training tasks and novel learning experiences stimulate the prefrontal cortex—similar to how resistance exercise stimulates muscle fibers.
This conceptual framework helps contextualize why a “workout” mentality benefits mental performance: consistent engagement in both physical activity and cognitively demanding tasks strengthens neural architecture in ways that improve function across domains.
Physical Exercise and Brain Health
Aerobic and Resistance Training
Physical exercise benefits the brain in ways that extend beyond weight management or cardiovascular health. Aerobic and resistance training have both been shown to facilitate neuroplasticity, improve connections between neurons, enhance blood flow, and stimulate the release of neurotrophic factors such as brain‑derived neurotrophic factor (BDNF), which supports neuronal survival and growth (Oyovwi et al., 2025). BDNF in particular plays a critical role in learning, memory, and mood regulation and is significantly increased following regular physical activity (Oyovwi et al., 2025).
Aerobic exercise—like walking, cycling, or swimming—increases cardiac output and delivers more oxygenated blood to the brain, enhancing cerebral perfusion and facilitating metabolic waste removal (Harvard Health, 2024). Resistance training, including weight lifting, has also been associated with improved executive function and memory in older adults, suggesting that muscular strength training may protect against age‑related cognitive decline (Harvard Health, 2025).
Intensity Matters but Any Movement Helps
Recent studies emphasize that physical activity need not be intense to benefit the brain. Even short bursts of brisk activity—such as walking fast enough that singing would be difficult—have been shown to reduce inflammation, improve blood flow, and promote neuroplasticity (Wisløff & Tari, 2025). These benefits extend to individuals across age groups and health statuses, and accumulating activity throughout the day can be particularly impactful.
Moreover, evidence suggests that strength training may help preserve brain volume and cognitive performance in aging adults diagnosed with mild cognitive impairment (Harvard Health, 2025). These findings underscore how structured physical activity serves as a protective factor against neurodegenerative processes and cognitive decline.
Mechanisms of Benefit
The neurobiological mechanisms linking exercise and brain health are multifaceted. They include:
- Increased neurotrophic factors: Exercise increases BDNF levels, which support cell survival and synaptic growth. Higher BDNF levels are associated with better memory and mood regulation (Oyovwi et al., 2025).
- Enhanced cerebral blood flow: Aerobic exercise increases blood flow to key memory and executive‑function areas like the hippocampus and prefrontal cortex (Harvard Health, 2024).
- Reduced inflammation and oxidative stress: Physical activity decreases systemic inflammation and enhances antioxidant defenses, which protect neurons from damage (Wisløff & Tari, 2025).
- Hormonal modulation: Exercise triggers neurochemical shifts—including increases in dopamine and endorphins—that support mood and cognitive performance (Harvard Health, 2024).
These pathways collectively demonstrate that physical activity strengthens the brain’s structural and functional resilience in ways that resemble—but do not literally replicate—muscle hypertrophy.
Cognitive “Workouts”: Mental Training and Learning Challenges
While physical exercise lays the groundwork for a healthy brain, cognitive exercise enhances its functional capacity. Cognitive tasks that challenge memory, problem‑solving, language, and spatial reasoning stimulate neural circuits, improving efficiency and adaptability. Activities like learning a new language, practicing musical instruments, engaging in complex games, or solving puzzles have been linked to enhanced cognitive reserves and delayed cognitive aging.
Although some commercial “brain training” programs vary in their efficacy, the underlying principle is supported by research: meaningful cognitive engagement fosters synaptic growth, improves connectivity between brain regions, and enhances neural efficiency (Pascual‑Leone et al., 2025). Pairing cognitive challenges with physical exercise compounds benefits because both approaches leverage neuroplasticity through unique but complementary mechanisms.
Mental Health Benefits of Exercise
Exercise and cognitive challenges also confer significant mental health advantages, which indirectly support brain function. Physical activity elevates mood, reduces symptoms of anxiety and depression, and improves self‑esteem—benefits mediated by neurochemical changes including increased endorphins, serotonin, and dopamine release. Regular movement also improves sleep quality, which is crucial for memory consolidation and emotional regulation.
These findings align with broader clinical evidence linking lifestyle interventions—including exercise, mindfulness, and cognitive engagement—to reduced symptoms of depression and anxiety and improved overall psychological resilience. Thus, moving one’s body and mind isn’t just “good for the brain”—it actively contributes to emotional well‑being.
Practical Strategies for Brain Workouts
Implementing a brain‑healthy routine need not be overwhelming. Below are evidence‑informed strategies:
- Aim for regular physical activity: Set achievable goals such as brisk walking, cycling, or dance classes 3–5 times a week. Even micro‑sessions of high‑intensity movement can be effective and easier to sustain.
- Incorporate strength training: Schedule resistance exercises twice weekly to support both muscular and neural health.
- Challenge your brain daily: Read complex material, learn new skills, or engage in intellectually demanding hobbies.
- Combine body and mind: Try mindful movement practices such as yoga, Tai Chi, or dance that require coordination, memory, and balance, which may yield cognitive benefits beyond traditional workouts.
- Stay socially engaged: Interaction with others provides emotional support and cognitive stimulation—key factors in long‑term brain health.
- Prioritize rest and recovery: The brain, like a muscle, requires rest. Quality sleep consolidates learning and fosters emotional regulation.
- Break up sedentary time: Long periods of inactivity may impair brain health independently of exercise, so frequent movement throughout the day matters (Verywell Health, 2025).
Conclusion
The analogy of the brain as a muscle is more than a catchy metaphor; it is a functional blueprint for lifelong brain health. While the brain is not composed of muscle tissue, it demonstrates remarkable adaptability in response to stimulation, exercise, and challenge. Physical activity promotes neuroplasticity, blood flow, and neurochemical support, while cognitive engagement strengthens neural connections, resilience, and functional capacity. Together, these approaches create a synergistic “workout” regimen that supports cognition, mood, immunity, and longevity.
Clinicians, caregivers, educators, and individuals should recognize that brain health is not static—it can be cultivated and strengthened throughout life. The science is clear: brains that are systematically challenged—both physically and cognitively—are more robust, adaptable, and resilient in the face of aging and stress. In this sense, working out isn’t just about muscles—it’s about empowering brains to grow stronger every day.
References
Harvard Health. (2024). Short‑term cognitive boost from exercise may last for many hours. Harvard Health Publishing. Harvard Health
Harvard Health. (2025). Weight training may protect the brain from cognitive decline. Harvard Health Publishing. Harvard Health
Oyovwi, M. O., Ogenma, U. T., & Onyenweny, A. (2025). Exploring the impact of exercise‑induced BDNF on neuroplasticity in neurodegenerative and neuropsychiatric conditions. Molecular Biology Reports. Springer
Pascual‑Leone, A., et al. (2025). The neuroplastic brain: current breakthroughs and emerging frontiers. Brain Research Reviews. ScienceDirect
Wisløff, U. & Tari, A. R. (2025). Small bursts, big gains: Exercise shields the aging brain. The Lancet summary. Neuroscience News
Verywell Health. (2025). Even if you exercise, sitting too much is bad for your brain. verywellhealth.com